|
Disclaimer: Information for research purposes only. Should you need medical treatment, seek the care of a qualified medical or complementary medicine practitioner. Herbal medicines have cautions, contraindications, and herb/drug interactions. Your individual risk factors should be assessed. Safety, quality, and efficacy are all important aspects of herbal medicine, and vary widely across the industry. Chinese medicine should always be used with the supervision of a licensed Chinese medicine practitioner. In no way does the information in this article attempt to diminish the helpfulness of Western antivirals when available and indicated. The U.S. has an FDA approved Paxlovid therapeutic treatment to prevent very serious illness when taken early. Ask your MD if you qualify for access. https://www.yalemedicine.org/news/13-things-to-know-paxlovid-covid-19. Some patients who experienced improvement of Covid-19 symptoms while under treatment of Paxlovid experienced a rebound effect. Scientists began working on the assumption that the dose and length of treatment may not have been sufficient for the viral load in these cases, despite high efficacy in preventing death. https://emergency.cdc.gov/han/2022/pdf/CDC_HAN_467.pdf. Sadly, not every country, nor every person in the U.S. has access to high quality Western treatment. Problems lacking health insurance or resources to access the U.S. healthcare system still abound in the United States. It is the opinion of this author that vaccines are helpful to both individuals and society as a whole, and none of the information regarding herbal medicine and supplements should be construed to be utilized in lieu of vaccination. https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-myths/art-20485720. Given the highly contagious BA.5 strain currently dominant, along with the debilitating severity of long-covid, efforts to prevent and mitigate risk are strongly indicated, especially since people can become reinfected with strains of Omicron as soon as four weeks after a previous infection. Single Herbs: Lysine, Qing Hao (Artemesia), over-the counter (OTC) immune-system agents (Zinc, Quinine, Quercetin, Vit E, Vit D3, Vit C), and Black Seed or Black Seed Oil have peer-reviewed evidence listed below (research highlighted is not exhaustive of the available research on these herbs). Other single herbs you may be interested in researching include: Lian Qiao (Forsythia), Jin Yin Hua (Flos Lonicerae Japonicae), Huang Qin (Radix Scutellariae), Da Qing Ye (Folium Isatidis), Cat’s Claw, Goldenseal (endangered). The single herbs above are not exhaustive of the herbs that can have an effect on SARS-CoV-2. In addition to the common herbs above, the following herbs can also act as agents that inhibit various pathways of SARS-CoV-2, reduce inflammatory cytokines, and reduce damage to lungs and tissues. Curcumin (Curcuma Longa L., Curcuma phaeocaulis Val.) (Jiang Huang, E Zhu), Citrus sinensis (Chen Pi), Diosmetin (Citrus aurantium L.) (Zhi Shi), Cimicifuga foetida L. (Sheng Ma), Melia azedarach L. (Ku Lian Pi), Coptis chinensis Franch (Huang Lian), Phellodendron chinense Schneid. (Huang Bai), and Sophora flavescens Ait. (Ku Shen), Rheum officinale Bail1. (Da Huang), Polygonum multiflorum Thunb. (He Shou Wu), and Caulis Polygoni multiflori (Shou Wu Teng), Sambucus williamsii Hance (Jie Gu Mu), Urtica fissa E. Pritz. (Xun Ma), Andrographis paniculata (Burm. f.) Nees (Chuan Xin Lian), Ephedra sinica Stapf. (Ma Huang)–Prunus armeniaca L. (Ku Xing Ren), Glycyrrhiza uralensis Fisch. (Gan Cao), Caffeic acid phenethyl ester (Cinnamomum cassia Presl.) (Rou Gui), Honokiol (Magnolia officinalis Rehd. et Wils.) (Hou Po), Cordyceps sinensis extract (Cordyceps sinensis (Berk.) Sacc.), Cordyceps sinensis extract (Cordyceps sinensis (Berk.) Sacc.), Ruscogenin (Ophiopogon japonicus (L.f) Ker-Gawl) (Mai Dong), Tanshinone IIA (Salvia miltiorrhiza Bge.) (Dan Shen), Isoforskolin (Sparganium stoloniferum Buch.-Ham.) (San Leng), Saikosaponins (Bupleurum chinense DC.) (Chai Hu). Chinese Medicine Formulas: The following Chinese medicine formulas have been studied extensively in multiple trials. Huoxiang Zhengqi Wan (Agastache Qi-Correcting Pills), Lianhua Qingwen Zhiji (Forsythiae and Honeysuckle Flower Pestilence-Clearing Preparations), ShufengJiedu Keli (Wind-Expelling and Toxin-Removing Granules), and Fangfeng Tongsheng Zhiji (Saposhnikoviae Heat-Clearing Preparations) Qingfei Paidu Tang (Lung-Cleansing and Toxins-Removing Decoction) (list not exhaustive, but indicative of the accepted protocol in China, after 7 trial iterations early in the pandemic). LYSINE: Lysine is an essential amino acid that has a long history of helping to suppress the herpes simplex virus (HSV) (herpes simplex 1 generally causes cold sores, herpes simplex 2 generally causes genital herpes, although some crossover can occur). The action of Lysine can be both inhibitory if taken preventatively, or can facilitate recovery during an outbreak. In contrast, the amino acid, Arginine, can feed the HSV, leading to outbreaks. L-Arginine is common in several different food categories. Occasionally, someone might be surprised at the outbreak of cold sores and then realize they recently began consuming large amounts of almond milk. Therefore, examining dietary triggers and aids can be helpful in suppressing viral load. To inhibit viral load, a person should consider increasing the ratio of Lysine to Arginine, but keep in mind that some of the same foods rich in Lysine are also rich in Arginine. Therefore, herbal supplement of Lysine may provide some benefit. Good sources of Lysine include foods that are rich in protein, such as:
Foods that are high in protein naturally contain L-Arginine including:
As you can see above, many of the same foods high in Lysine are also high in Arginine. Seeking a higher Lysine to Arginine ratio is desired to suppress viral activity (example: Fenugreek seed). For this reason, supplemental Lysine is sometimes helpful. If you do take a supplement, I recommend high quality vegetarian capsules, without fillers or stearate as binders. (available on https://wellevate.me/Innovations-to-Wellness for 10% off MSRP) LYSINE and SARS-CoV-2 How does Lysine interact with Covid-19? In the peer-reviewed, evidence-based journal of Viruses, one study found that Lysine can inhibit the virus at early stages of SARS-CoV-2 and may act as a helpful supplement in prevention. These authors confirmed the finding re: Arginine and Herpes in relation to other viruses like Covid-19 and Influenza A (Arginine increases the activity of Covid-19 and Influenza A (IAV)). Therefore, while Lysine appears to inhibit viral activity, Arginine appears to increase viral loads. Melano I, Kuo LL, Lo YC, Sung PW, Tien N, and Su WC, Effects of Basic Amino Acids and Their Derivatives on SARS-CoV-2 and Influenza-A Virus Infection. Viruses. 2021 Jul: 13(7): 1301. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8310019/#:~:text=Lysine%20and%20Lys%2Dester%20can,COVID%2D19%20and%20flu%20patients. These authors found that Lysine could reduce viral load, showing that: “Lysine and Lys-ester can attenuate SARS-CoV-2 infection in the cell culture system (Figure 2A). Consistent with a previous study, IAV replication was also inhibited by lysine (Figure 4) [20]. Lysine therapy has long been recommended against HSV infection because it can suppress viral replication and inhibit virus yield [23,26,27,28,38].” “Possible mechanisms for the suppressing of SARS-CoV-2 could occur at the fusion peptide and endosomal membrane, potentially disrupting the release of virus particles. Another possible mechanism could result from lysine’s ability to reduce intracellular calcium levels. The authors conclude that, L-“Lysine and Lys-ester can prevent SARS-CoV-2 and IAV infection, particularly in the entry stage. In contrast to that, Arg-ester can potently boost infection of both viruses. It would therefore be beneficial to consider the nutrient intake of COVID-19 and flu patients.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8310019/#:~:text=Lysine%20and%20Lys%2Dester%20can,COVID%2D19%20and%20flu%20patients. These author’s findings reinforce the protective effect of looking at your dietary intake in addition to possible recommendations of Lysine supplementation in both prevention and early treatment of Covid-19. Decreasing Arginine intake is also important. While Lysine demonstrates good effect among early, mild, and moderate Covid, L-Lysine should be used with caution among patients with severe Covid, at least those with high fever. https://www.science.org/do/10.1126/comment.742380/full/ Zinc: (available on https://wellevate.me/Innovations-to-Wellness 10% off MSRP)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8310019/#:~:text=Lysine%20and%20Lys%2Dester%20can,COVID%2D19%20and%20flu%20patients. Caution in taking Zinc at high levels, as toxicity can occur from excessive doses. Take only at approved levels. Quinine water is readily available in the United States. For safe sourcing of Quinine, see original article.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8310019/#:~:text=Lysine%20and%20Lys%2Dester%20can,COVID%2D19%20and%20flu%20patients.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8310019/#:~:text=Lysine%20and%20Lys%2Dester%20can,COVID%2D19%20and%20flu%20patients.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8310019/#:~:text=Lysine%20and%20Lys%2Dester%20can,COVID%2D19%20and%20flu%20patients. Vitamin K2/D3: (K2 helps with D3 absorption - available for 10% off MSRP on https://wellevate.me/Innovations-to-Wellness)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8310019/#:~:text=Lysine%20and%20Lys%2Dester%20can,COVID%2D19%20and%20flu%20patients.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8310019/#:~:text=Lysine%20and%20Lys%2Dester%20can,COVID%2D19%20and%20flu%20patients.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8310019/#:~:text=Lysine%20and%20Lys%2Dester%20can,COVID%2D19%20and%20flu%20patients. The authors of “Effects of Basic Amino Acids and Their Derivatives on SARS-CoV-2 and Influenza-A Virus Infection” found a strong statistical significance in favor of the effectiveness of the above OTC formulations “for prevention and treatment of (retro)viral infections, inclusive of COVID-19, over a 20-week period”, even when adopting low assumptions/estimates for the widespread Covid-19 virus spread patterns during the time of the study. For citations within text, more information re: methods, study design, and analysis, please see original article in Journal of Evidence-Based Integrative Medicine. https://journals.sagepub.com/doi/pdf/10.1177/2515690X211026193 Qing Hao (Artemesia, a commonly used treatment for malaria) and SARS-CoV-2 Qing Hao (Artemesia) has received widespread acknowledgement in the treatment of malaria since at least 2001, when it was recognized by the WHO. But how does it interact with Covid-19? Artemisia was utilized in 2003 during the SARS-CoV-1 outbreak, and scientists recently studied its impact on SARS-CoV-2. Law S, “Is the Traditional Chinese Herb Artemisia annua possible to fight against Covid-19?”, Integr Med Res. 2020: Sept; 9(3): 100474. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7362865/
Limitations of Qing Hao:
Qing Hao must be carefully sourced for quality and safety and is not as ubiquitously available as Lysine. In Chinese medicine, Qing Hao is not usually utilized in isolation, but in balanced formulas that treat holistically. Additional resources studying the impact of Qing Hao (Artemisia annua) can be found here: Fuzimoto A. “An Overview of the anti-SARS-CoV-2 properties of Artemisia annua, its antiviral action, protein-associated mechanisms, and repurposing for COVID-19 treatment.” J Integr Med. 2021 Sep. and here: “The combination of A. annua's biological properties, action on different signaling pathways and target proteins, and a multi-drug combined-therapy approach may synergistically inhibit SARS-CoV-2 and assist in the COVID-19 treatment. Also, A. annua may modulate the host immune response to better fight the infection.” https://pubmed.ncbi.nlm.nih.gov/34479848/#:~:text=annua's%20biological%20properties%2C%20action%20on,to%20better%20fight%20the%20infection Black Seed or Black Seed Oil (Nigella Sativa), also called Black Cumin Seeds Khazdair MR, Ghafari S, Sadeghi M. “Possible therapeutic effects of Nigella Sativa and its thymoquinone on Covid-19.” Pharm Biol. 2021; 59(1): 696–703. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8204995/ These authors investigated the mechanisms involved with Black Seed or Black Seed Oil (Nigella Sativa) finding evidence to support that “N. sativa and TQ reduced the level of pro-inflammatory mediators including, IL-2, IL-4, IL-6, and IL-12, while enhancing IFN-γ. Nigella sativa and TQ increased the serum levels of IgG1 and IgG2a, and improved pulmonary function tests in restrictive respiratory disorders.” They concluded that “N. sativa and TQ might have beneficial effects on the treatment or control of COVID-19 due to antiviral, anti-inflammatory and immunomodulatory properties as well as bronchodilatory effects”, encouraging additional clinical studies. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8204995/ Three additional resources investigating the role of Black Cumin Seeds in potential therapeutic effect on Covid-19 include:
These articles just scratch the surface on studies done on Black Seed. A quick peer-reviewed search includes many others, including, but not limited to: Thymoquinone’s Antiviral Effects: It is Time to Be Proven in the Covid-19 Pandemic Era and Its Omicron Variant Surge. https://www.frontiersin.org/articles/10.3389/fphar.2022.848676/full and: Antiviral effects of black seeds: Effect on COVID-19. https://www.sciencedirect.com › science › article › pii Chinese Medicine Formulas and Covid-19: All of the examples above have been presented in Western fashion, as separate herbs, with an examination of the function and mechanism of each independently. However, in the application of Chinese medicine, herbal supplements are rarely used in isolation, but rather in balanced formulas, used in conjunction with other herbs. Chinese medicine formulas are paired with the extensive diagnostic pattern differentiation process, applied based on signs/symptoms, asking questions, looking (tongue diagnosis, color, etc), listening, and palpation (e.g. feeling pulse - see this post for an introductory glimpse into the art of Chinese pulse palpation) http://www.innovationstowellness.com/blog/chinese-pulse-diagnosis-the-art-of-palpation. The treatment of Covid-19 with Chinese medicine both overlaps pharmacologically with Western medicine, but also extends into the long-tested clinical traditions of Chinese medicine.
These ancient guidelines are similar to the modern day strategies of epidemiology and public health prevention to minimize the impact of epidemics and pandemics. However, the method of treatment in Chinese medicine retains unique adherence to a holistic view, rather than solely a mechanistic method.
The authors of this article, Ni et al. “Combating Covid-19 with Integrated Traditional Chinese and Western Medicine in China.” Acta Pharm Sin B. 2020 Jul: 10(7):1149-1162. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7319939/, go into great detail on the application of several Chinese medicine formulas implemented to treat Covid-19 early in the pandemic, before vaccines were available. I highly recommend reading it in its entirely if you are interested in the mechanisms and pathopharmacology of the formula interventions. Three patent medicines were initially studied: (Lianhua Qingwen Keli/Jiaonang (Forsythiae and Honeysuckle Flower Pestilence-Clearing Granules/Capsules), Jinhua Qinggan Keli. In trial version 4, the study examined: (Huoxiang Zhengqi Wan (Agastache Qi-Correcting Pills), Lianhua Qingwen Zhiji (Forsythiae and Honeysuckle Flower Pestilence-Clearing Preparations), Shufeng Jiedu Keli (Wind-Expelling and Toxin-Removing Granules), and Fangfeng Tongsheng Zhiji (Saposhnikoviae Heat-Clearing Preparations) In trial version 6 and 7, the specific protocol recommendation included: “Qingfei Paidu Tang (Lung-Cleansing and Toxins-Removing Decoction), along with modified formulas for different stages (mild, moderate, severe, critical, and convalescence). In addition, Fangfeng Tongsheng Zhiji was removed from the recommended lists of Chinese patent medicine (Table 2).” At the time of publication of the above article, April 2020, an evidence-base had already begun to be established:
Initial application of Chinese medicine formulas began with the history of treatment of SARS in late 2002, 2003.(44). Research demonstrated that while different from the specifically targeted activities of Western medications.
In addition to the broad antiviral effects, TCM treatment addresses the massive inflammatory pathway in conjunction with immune system regulation and promoting healing.
Therefore, the Lianhua Qingwen Capsules studied appeared to have antiviral effects, anti-inflammatory mechanisms, and immune-system modulation in their therapeutic activity. Other formulas also have multiple pathways towards healing.
Excerpts have been presented above, for the complete study, please see all of the data here: Ni L, Chen L, Huang X, Han C, Xu J, Zhang H, Luan X, Zhao Y, Xu J, Yuan W, Chen H. “Combating Covid-19 with Integrated Traditional Chinese and Western Medicine in China.” Acta Pharm Sin B. 2020 Jul: 10(7):1149-1162. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7319939/ Despite the substantial and far-reaching implications of the treatment of Covid-19 with Chinese medicine, as evidenced by the various pathways, mechanisms, and broad inflammatory reduction and immune-boosting actions of the formulas outlined in the article above, some limitations for their use exist specifically within the United States, because of the inclusion of Ma Huang in many of the above verified treatments for Covid-19. Ma Huang (a particularly important herb used in the treatment of lung conditions, channel obstruction, colds and flus) was misused by Western pharmaceutical companies in dangerous ways and subsequently banned for use in the United States. Ma Huang is contraindicated for sweating, cardiovascular disorders, and high blood pressure; common contraindications learned during the 3-4 years of intensive training received by Chinese medicine students in the United States. Ma Huang should not be combined with other stimulants, should be cooked appropriately (at least 45 minutes, draining and discarding the froth off from the top), and should be monitored carefully with only short-term use. Instead of being utilized safely, within the safety and preparation methods utilized in Chinese medicinal use, the components in Ma Huang were taken out of its safely monitored Chinese medicinal use context and were used inappropriately, as highly concentrated ephedra and promoted in opposition to its contraindications as a weight loss drug -which it is not a Chinese medicinal indication for Ma Huang-it is indicated to support the lungs or certain types of pain in Chinese medicine). https://www.pacificcollege.edu/news/blog/2014/07/07/ma-huang-herb-misused-and-abused As a result of the FDA ban on Ma Huang, practitioners in the United States are not allowed to use it safely for its intended use to support the lungs. As a result, many of the formulas for treating Covid-19 listed above must be modified, and equivalent research and data without the use of Ma Huang is not available. Modifications are frequently used by Chinese medicine practitioners, as formulas are often tailored for an individuals’ signs/symptoms, pattern; however, the efficacy of Ma Huang replacements are not identical. Pharmacokinetic Properties of Chinese Medicine on SARS-CoV-2 Li L, Wu Y, Wang J, Yan H, Lu J, Wan Y, Zhang B, Zhang J, Yang J, Wang X, Zhang M, Li Y, Miao L, and Zhang H. “Potential Treatment of COV ID-19 with Traditional Chinese Medicine: What Herbs Can Help Win the Battle with SARs-CoV-2?” Engineering. 2021: Oct 28. Doi: 10.1016/j.eng.2021.08.020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8552808/ The authors above found inhibitory effects on SARS-CoV-2 and sequelae by single herbs that included: Curcumin (Curcuma Longa L., Curcuma phaeocaulis Val.) (Jiang Huang, E Zhu), Citrus sinensis (Chen Pi), Diosmetin (Citrus aurantium L.) (Zhi Shi), Cimicifuga foetida L. (Sheng Ma), Melia azedarach L. (Ku Lian Pi), Coptis chinensis Franch (Huang Lian), Phellodendron chinense Schneid. (Huang Bai), and Sophora flavescens Ait. (Ku Shen), Rheum officinale Bail1. (Da Huang), Polygonum multiflorum Thunb. (He Shou Wu), and Caulis Polygoni multiflori (Shou Wu Teng), Sambucus williamsii Hance (Jie Gu Mu), Urtica fissa E. Pritz. (Xun Ma), Andrographis paniculata (Burm. f.) Nees (Chuan Xin Lian), Ephedra sinica Stapf. (Ma Huang)–Prunus armeniaca L. (Ku Xing Ren), Glycyrrhiza uralensis Fisch. (Gan Cao), Caffeic acid phenethyl ester (Cinnamomum cassia Presl.) (Rou Gui), Honokiol (Magnolia officinalis Rehd. et Wils.) (Hou Po), Cordyceps sinensis extract (Cordyceps sinensis (Berk.) Sacc.), Cordyceps sinensis extract (Cordyceps sinensis (Berk.) Sacc.), Ruscogenin (Ophiopogon japonicus (L.f) Ker-Gawl) (Mai Dong), Tanshinone IIA (Salvia miltiorrhiza Bge.) (Dan Shen), Isoforskolin (Sparganium stoloniferum Buch.-Ham.) (San Leng), Saikosaponins (Bupleurum chinense DC.) (Chai Hu). The formulas Li et al. tested and found to have inhibitory effects on SARS-CoV-2 included: Qingfei Paidu decoction (QFPD), the Huashi Baidu formula (HSBD), Ma Xing Shi Gan decoction (MXSGD) the Xuanfei Baidu decoction (XFBD), the Jinhua Qinggan granule, the Lianhua Qingwen capsule/granule (LHQW), and the Xuebijing injection (XBJ). For a complete list of compounds, specific pathways of interaction, and pharmacokinetic data investigated, please see the authors’ original article here: Li L, Wu Y, Wang J, Yan H, Lu J, Wan Y, Zhang B, Zhang J, Yang J, Wang X, Zhang M, Li Y, Miao L, and Zhang H. “Potential Treatment of COV ID-19 with Traditional Chinese Medicine: What Herbs Can Help Win the Battle with SARs-CoV-2?” Engineering. 2021: Oct 28. Doi: 10.1016/j.eng.2021.08.020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8552808/ Li et al. first outline the mechanisms of Covid-19:
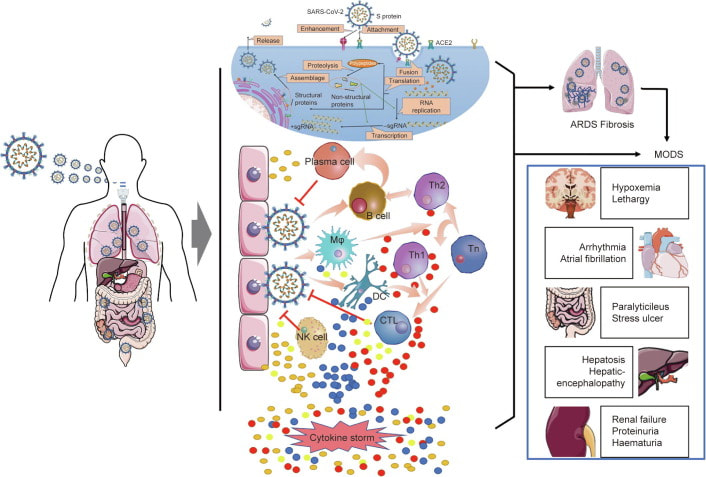
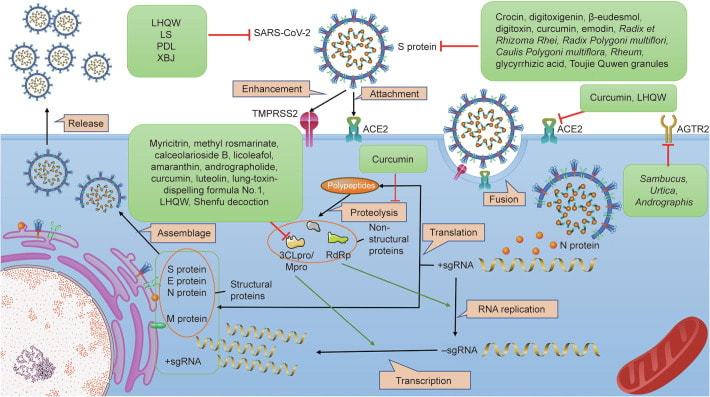
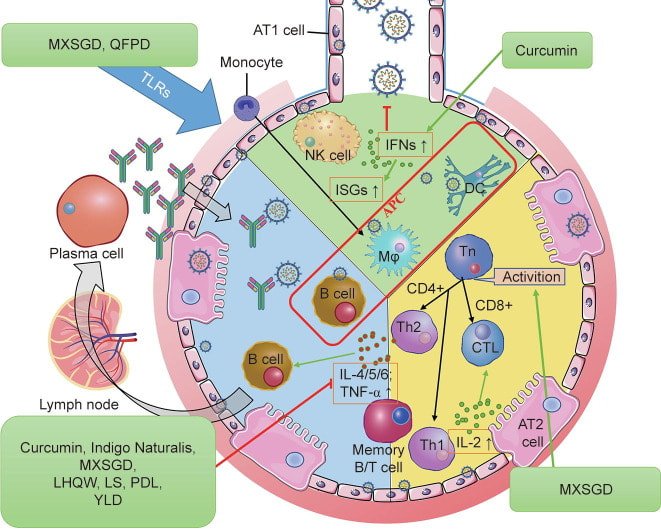
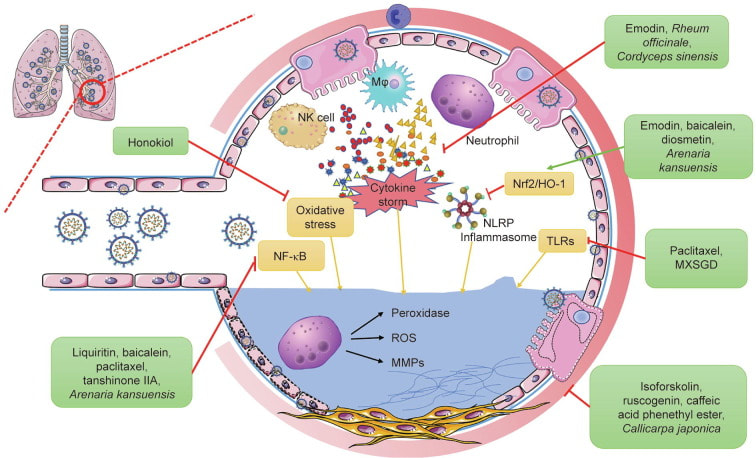
“Figure 1: Pathogenesis of COVID-19. After entering the human body, SARS-CoV-2 invades cells by binding with ACE2 and begins to replicate in the cytoplasm of the host cells. The virus is presented to B and T cells by macrophages and dendritic cells, while the host immune system is simultaneously activated. B and T cells are differentiated into effector immune cells, inducing the production of proinflammatory cytokines and chemokines. However, continuous activation of the immune system and accumulation of cytokines can lead to uncontrolled cytokine storm, causing the lungs and other organs to be seriously injured by SARS-CoV-2 infection. MODS: multiple organ dysfunction syndrome; TMPRSS2: transmembrane protease serine 2; Th: T helper cell; CTL: cytotoxic T lymphocyte; DC: dendritic cell; NK: natural killer; Tn: naive T cell; Mφ: macrophage.” Li L, Wu Y, Wang J, Yan H, Lu J, Wan Y, Zhang B, Zhang J, Yang J, Wang X, Zhang M, Li Y, Miao L, and Zhang H. “Potential Treatment of COV ID-19 with Traditional Chinese Medicine: What Herbs Can Help Win the Battle with SARs-CoV-2?” Engineering. 2021: Oct 28. Doi: 10.1016/j.eng.2021.08.020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8552808/ For a complete list of compounds, specific pathways of interaction, and pharmacokinetic data investigated, please see the authors’ original article. “Figure 2: Antiviral action by TCM. TCM inhibits infection of SARS-CoV-2 through multiple mechanisms, including prevention of the activity of ACE2 and the S protein by directly binding with them, downregulating the expression of the receptors of the S protein (e.g., ACE2 and angiotensin II receptor type 2 (AGTR2)), and inhibiting viral replication by suppressing the expression of RdRP and 3CLpro. The representative TCMs related to each mechanisms are listed in the green boxes. Mpro: main protease; sgRNA: single guide RNA.” Li L, Wu Y, Wang J, Yan H, Lu J, Wan Y, Zhang B, Zhang J, Yang J, Wang X, Zhang M, Li Y, Miao L, and Zhang H. “Potential Treatment of COV ID-19 with Traditional Chinese Medicine: What Herbs Can Help Win the Battle with SARs-CoV-2?” Engineering. 2021: Oct 28. Doi: 10.1016/j.eng.2021.08.020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8552808/ For a complete list of compounds, specific pathways of interaction, and pharmacokinetic data investigated, please see the authors’ original article. These authors also documented the anti-inflammatory mechanisms of TCM on the immune system. “Figure 3: TCM immune modulation and anti-inflammation. TCM treats SARS-CoV-2 infection by modulating the host immune system, which includes increasing the production of interferons (IFNs) at the onset of the disease, inhibiting Toll-like receptor (TLR)-mediated inflammatory response, suppressing the production of proinflammatory cytokines, and inducing the differentiation of T and B cells into effector immune cells. The representative TCMs acting on each pathway are listed in the green boxes. CD: cluster of differentiation; ISG: interferon-stimulated gene; AT: alveolar type.” Li L, Wu Y, Wang J, Yan H, Lu J, Wan Y, Zhang B, Zhang J, Yang J, Wang X, Zhang M, Li Y, Miao L, and Zhang H. “Potential Treatment of COV ID-19 with Traditional Chinese Medicine: What Herbs Can Help Win the Battle with SARs-CoV-2?” Engineering. 2021: Oct 28. Doi: 10.1016/j.eng.2021.08.020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8552808/ For a complete list of compounds, specific pathways of interaction, and pharmacokinetic data investigated, please see the authors’ original article. The authors continued to investigate the influence on lung deterioration related to Covid-19 and found protective effects within the lungs as well. “Figure 4: Suppression of lung injury and fibrosis by TCM. TCM reduces lung injury and pulmonary fibrosis by inhibiting inflammation-related and oxidation-related pathways, such as by downregulating the expression of cytokines, inflammasomes, and reactive oxygen species (ROS); suppressing alveolar neutrophil infiltration; inhibiting NF-κB, nuclear factor E2-related factor 2 (Nrf2)/heme oxygenase-1 (HO-1), and TLR-mediated pathways; and reducing oxidative stress. The representative TCMs acting through each pathway are listed in the green boxes. NLRP: nucleotide-binding domain leucine-rich repeat (NLR) and pyrin domain containing receptor; MMP: matrix metalloproteinase.” Li L, Wu Y, Wang J, Yan H, Lu J, Wan Y, Zhang B, Zhang J, Yang J, Wang X, Zhang M, Li Y, Miao L, and Zhang H. “Potential Treatment of COV ID-19 with Traditional Chinese Medicine: What Herbs Can Help Win the Battle with SARs-CoV-2?” Engineering. 2021: Oct 28. Doi: 10.1016/j.eng.2021.08.020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8552808/ For a complete list of compounds, specific pathways of interaction, and pharmacokinetic data investigated, please see the authors’ original article. As you can see from the very brief overview of highlighted single herbs and herbal formulas above, the peer-reviewed evidence base for the use of herbal treatments as therapeutics and in treatment of the negative sequelae for the damage caused by Covid-19 is quite extensive. As more research articles are funded and executed, more evidence on the helpfulness of complementary medicine in conjunction with Western therapeutics is likely. Given the extensive and continuing widespread community exposure worldwide and the devastating effects people have reported suffering from long-Covid, it is useful to examine and research all methods available for helping the health of individuals and entire population groups improve. Disclaimer: Information for research purposes only. Should you need medical treatment, seek the care of a qualified medical or complementary medicine practitioner. Herbal medicines have cautions, contraindications, herb/drug interactions, and your individual risk factors should be assessed. Safety, quality, and efficacy are all important aspects of herbal medicine, and vary widely across the industry. In my opinion, the Australian standards on herbal medicine are excellent. https://www.tga.gov.au/overview-regulation-complementary-medicines-australia https://www.tga.gov.au/sites/default/files/australian-regulatory-guidelines-complementary-medicines-argcm.pdf In California, prop 65 mandates that herbal medicine must be labeled as “potentially causing cancer, birth defects, or other reproductive harm” regardless of adherence to prop 65 standards. Mayway, one of several supplies of Chinese herbal medicine in the United States adheres to the highest standards for testing in heavy metals, toxicity, and safety. In addition to complying with prop 65, their Plum Flower line also adheres to the Australian good manufacturing practice (GMP) standards for strict quality control, certified GMP. https://www.mayway.com/education/patient-education/pamphlet-heavy-metals-chinese-herbs-proposition-65-english In no way does the information in this article attempt to diminish the helpfulness of Western antivirals when available and indicated. The U.S. has an FDA approved Paxlovid therapeutic treatment to prevent very serious illness when taken early. Ask your MD if you qualify for access. https://www.yalemedicine.org/news/13-things-to-know-paxlovid-covid-19. Some patients who experienced improvement of Covid-19 symptoms while under treatment of Paxlovid experienced a rebound effect. Scientists began working on the assumption that the dose and length of treatment may not have been sufficient for the viral load in these cases, despite high efficacy in preventing death. https://emergency.cdc.gov/han/2022/pdf/CDC_HAN_467.pdf. Sadly, not every country, nor every person in the U.S. has access to high quality Western treatment. Problems lacking health insurance or resources to access the U.S. healthcare system still abound in the United States. It is the opinion of this author that vaccines are helpful to both individuals and society as a whole, and none of the information regarding herbal medicine and supplements should be construed to be utilized in lieu of vaccination. https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-myths/art-20485720. Given the highly contagious BA.5 strain currently dominant, along with the debilitating severity of long-covid, efforts to prevent risk are indicated.
1 Comment
Before I decided to transition from a public health policy researcher to learn Chinese medicine, I read an article written by an old cardiologist lamenting the lost art of pulse diagnosis in even a Western framework context in favor of expensive albeit precise tests and monitoring available in modern Western medicine. In his article, he compared the type of care available in the U.S. and the subsequent lost skills of Western M.D.s to his counterparts in Africa, who utilized much more sophisticated methods of palpation-based pulse diagnosis to assess a range of heart conditions. Without the expensive equipment that also posed portability issues, African doctors were able to diagnose a range of heart conditions by pulse and intake examination, skills that he noted had been lost in the U.S. during his long career as a cardiologist near his retirement. This cardiologist also discussed the disparities in the U.S. healthcare system, with access to expensive ranges of tests resting almost solely with the insured population, with notably reduced access among the uninsured and poorer patients. I wish I had kept the article (I cannot now find the original), but the idea persisted in the background of my mind, when I came across a pulse map (like Figure 1 below) for the first time. As a Western public health researcher, I was fascinated by the idea of six pulse positions, multiple depths, and over 28 pulse qualities. 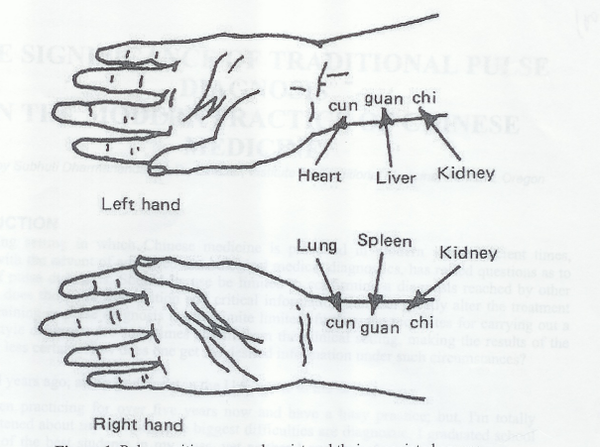 Figure 1: Anson Chui Yan Tang, Pulse Map: Review of Traditional Chinese Medicine Pulse Diagnosis Quantification Early into my Chinese medicine studies, I had the good fortune in being trained briefly by Dr. Robert Johns, O.M.D (https://www.johnsomd.com/), who trained extensively with the famous Chinese medicine Dr. Shen (pulse diagnosis book available here: https://www.amazon.com/Handbook-Contemporary-Chinese-Pulse-Diagnosis/dp/0939616769 and Chinese herbal medicine book available here: https://www.amazon.com/Chinese-Herbal-Medicine-Formulas-2012-12-05/dp/B01FIY6RUO). Dr. Johns described the deep impact of his studies with Dr. Shen, outlining that over 30 heart conditions can be assessed and diagnosed by careful evaluation of pulse examination, with sufficient training and experience. This concept reinforced my first exposure to the idea from the cardiologist’s article, and I was later able to receive additional training from Dr. Will Morris, DAOM, PhD (see below), who also trained in Dr. Shen’s tradition. What does all this detailed pulse information mean for you? While some exceptions for classical and detailed practitioner understanding occur (such as deeper in the kidney pulse, more superficial in the lung/heart positions), ideally, you would like to observe some balance between all six positions. Try feeling your pulse right now. Start by putting three fingers down on the radial pulse, beginning at the wrist crease (see Figure 1). Don’t overthink it, just place your fingers. What do you feel? Does anything stick out to you? Don’t get bogged down in different kinds of qualities, just observe what you can tell in your initial impression. Can you feel the rate? Is it fast or slow or average? Do you feel any pulse location very strong or very weak relative to the others? Is it stronger on the left or the right compared to the other side? Take a moment to just jot down your first impression of your own pulse. Having a basic impression of the overall relative balance between the six positions gives you a great start for avenues that might guide your meditation practice or self-care moxibustion/acupressure, even nutritional and dietary support. You may find it interesting and helpful to observe your pulse over time and in different situations, for example, just after a stressful event, in very hot or cold conditions, or when you’ve just experienced something happy and peaceful. Use what you observe to assist in your journey of self-discovery and finding balance in your day-to-day life. For more detailed support, you may wish to seek out a Chinese medicine practitioner. Chinese pulse diagnosis overview: Pulse diagnosis involves feeling the quality of the pulse at at six different positions on the radial pulse area (corresponding to Heart, Liver, Kidney Yin from distal to proximal on the left and Lung, Spleen(St), Kidney Yang from distal to proximal on the right). (https://www.sciencedirect.com/topics/medicine-and-dentistry/pulse-diagnosis) . The following open source chapter goes into great detail describing Chinese pulse diagnosis (see also Figure 1 above). Chui Yan Tang, Anson. Review of Traditional Chinese Medicine Pulse Diagnosis Quantification. October 17, 2012. In Complementary Therapies for the Contemporary Healthcare, Ed: Saad, Marcela and Medeiros, Roberta. https://www.intechopen.com/chapters/40015. In addition to observation of the simple pulse rate, approximately 28 different qualities are commonly observed and used in modern pulse diagnosis. The ancient Chinese medical classics, like the NeiJing, identify 30 pulse qualities. My first pulse teacher, Dr. Denise Hsu, had us take hundreds of pulses when we were just learning pulses for the first time. She made empty paper charts of the six positions for us to document practicing pulse examination on all our friends/family members/school clinic clients, jotting down our initial impressions of the pulse qualities at all six positions. As our practice extended, so did our sophistication with assessing the various pulse qualities. In addition to quantity (pulse rate) and quality (usually 28 qualities commonly used), various depths are also used in diagnostic methods. In some traditions, a practitioner feels for superficial and deep levels. In other traditions, practitioners feel for the different qualities at three depths: superficial, medium, and deep. The qualities may differ at the different depths, corresponding to disharmonies within the body and energetic imbalance. More involved pulse specialists like Dr. Will Morris, DAOM, PhD, teach that additional qualities can be felt for the intestines and other organ systems (Figure 2) in the in between spaces (can read more from Will Morris in his book Neoclassical Pulse Diagnosis available here: https://www.amazon.com/Neoclassical-Pulse-Diagnosis-William-Morris/dp/1641849347) and here, Li-Shi-Zen’s Pulse Studies: https://www.amazon.com/Li-Shi-Zhens-Pulse-Studies-Illustrated/dp/7117137622/ref=sr_1_1?crid=1UBNVVJNROF0H&keywords=li+shi-zhen%27s+pulse+studies&qid=1658255638&s=books&sprefix=li+shi-zhen%27s+pulse+studies%2Cstripbooks%2C149&sr=1-1. Figure 2: Will Morris, Pulse Map: Neoclassical Pulse Diagnosis Although Classically, different pulse qualities are felt during different seasons (i.e. more superficial in summer when the Qi rises to the surface, or deep in the winter when the Qi dives deeper into the body), our post-industrial society especially in the last decade has seen a divergence from harmony of people’s pulses with the seasonal influence, noted by some of the more famous Chinese medical doctors like Giovanni Maciocia (podcast) and Dr. Will Morris (workshop).
Below are some pulse-taking details that you may find interesting: Lonny Jarret writes in Nourishing Destinies: The Inner Tradition of Chinese Medicine (Spirit Path Press, 2015 (https://www.spiritpathpress.com/) that if the pulse is stronger on the right side (lung, spleen, kidney yang), the body is expending the original source Qi (pre-natal) treasures from heaven, a finite supply (Jing (essence), Qi, Shen (spirit)), consuming post-natal Jing, Qi, and Shen to compensate. This effect happens commonly among people who overwork (overwork is a common source of disease in Chinese medicine, overconsuming one’s inherent resources). “The pulses of the left hand correspond fundamentally to the quality of the function of the organ systems themselves, which finds its basis in the kidney. The right hand pulses correspond to the digestive system. If the pulses on the right hand are significantly better in quality and quantity than the left hand, then we may surmise that the actual functioning of the organ systems has collapsed. This collapse suggests that the resources of jing, Qi, and shen, have been severely depleted and are compromised as guiding influences in life. In this case, the digestive system is compensating and overworking in order to extract the maximum amount of essence from food and air so it may support the continued functioning of the organism. The collapse of the organ system corresponds to the compromised function of the mingmen [gate of fire], which plays a key role in guarding the inherited constitution.” Lonny Jarrett, Nourishing Destinies, p.112. Dr. Will Morris teaches that the left proximal pulse (kidney yin) can also be used to assess ancestral information (a skilled practitioner can help address familial issues by utilizing this method). The left middle pulse (liver position) sometimes is not felt when pressing all the way down to the deepest level - this is called “no root”, and can often be helped by taking Astragalus (Huang Qi), a superior class of herb (see your practitioner for cautions, contraindications, dosage, any possible herb/drug interactions*). A fast or wiry pulse in the liver position may also indicate stress, whereas a thready pulse may indicate blood deficiency (blood deficiency can often be detected before Western tests show full-blown anemia, an excellent avenue for prevention). In Japanese acupuncture and contact needling methods of treatment, the pulse is taken frequently throughout the entire treatment, observing the changes to the pulse and making subtle adjustments to improve balance. Pulse changes can occur quickly, whereas tongue diagnosis changes more slowly. Therefore, the effectiveness of the treatment can easily be observed by the qualitative and quantitative pulse changes during the session. Pulse examination can be highly detailed or observed at a simple overview of impressions to facilitate your journey to achieving greater balance in your life, your health, and your physical systems. Whatever entry point you wish to discover in pulse examination, a deeper dive is always possible. *FDA Disclaimer: No curative claims are being made regarding the properties of herbal medicine or pulse examination. Information is provided for research only. For specific health needs, please consult a qualified practitioner to ensure safety and assess any cautions, contraindications, or herb/drug interactions. You may also enjoy these articles: The Pulse in Ancient Medicine: Part 1: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5965015/ The Pulse in Medieval and Arab-Islamic Medicine: Part 2: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6219283/ The Pulse from Ancient to Modern Medicine: Part 3: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6448473/ How Does Pulse Diagnosis Work? https://www.dc-acupuncture.com/physical-health/how-pulse-diagnosis-works A Brief Journey into the History of the Arterial Pulse: https://www.hindawi.com/journals/crp/2011/164832/ Past, Present, and Future of the Pulse Examination (Mai Zhen): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3942893/ The Lost Art of the Physical Exam: https://medicine.yale.edu/news/yale-medicine-magazine/article/the-lost-art-of-the-physical-exam/ |
AuthorDr. Crystal Lynn Keeler has studied public health and health policy research for two decades and has been practicing Chinese medicine since 2012. Well-versed in healthy balance, meditation, seeking a joyful life, and helping others, Dr. Crystal hopes to inspire you on your healing path. ArchivesCategories |







 RSS Feed
RSS Feed
